Playing The Hand I Was Dealt
Surviving Keratoconus & A Body Falling To Pieces
Tag Archives: CXL
18 MONTHS AFTER CXL & THE MONKEYS SCRATCHING THEIR HEADS
Image Source: http://www.buddhaweekly.com
A decade or so before my keratoconus showed up, I recall seeing my former internist back home when I became so horrible ill from what I now know was classical Ehlers-Danlos syndrome. I had lost 30 lbs and was well below 100 due to throwing up from the pain all day and had this gaunt face with dark under eye circles when my doctor walked into the exam room and said to the half-dead person in front of him, “What happened to you?” in a very concerned tone. My internist was a smart and good doctor, but he was scratching his head like a monkey over what could possibly have made a fit and healthy young woman turn into a zombie seemingly overnight. In the end, he ordered blood work and sent me a copy with a referral to a rheumatologist. My doctor hand wrote the following on my report: You look good on paper.
I happened to have my annual eye exam this week and it’s been about 18 months since I had bilateral collagen cross-linking (CXL) to hopefully halt the progression of my keratoconus (KC), as well. The majority of the side effects from CXL have not gone away, and I still have the odd, right eye that originally got 6 lines of visual acuity (VA) back and then started to lose vision last October. I was sure the KC was back and had seen my optometrist to figure out what was going on, but my topographies were unchanged, which left him scratching his head like a monkey and then swearing, which was a first. That exciting appointment is detailed in this post.
The vision in my right eye has become even more ghosted recently and the prescription in my right scleral lens that I need to wear to drive is not correcting the ghosting anymore, so I figured I’d have my ophthalmologist redo my topographies to hopefully shed some light on the problem. After all, two heads are better than one and both my optometrist and ophthalmologist are well-versed in keratoconus and Ehlers-Danlos. For those who know my KC ordeal, this is my dry eye specialist who I actually like as I fired the inept corneal specialist 6 months ago. Good riddance.
Once again, I found out that there is no progression of the keratoconus in either eye, although the cone on my left cornea was blasted off during CXL for some odd reason and my scan still shows no keratoconus, although the resulting scar, or corneal opacity, has resulted in keratoconic vision in that eye that can’t be fully corrected. My doctor checked the opacity for progression and it’s the same, but he said that I had something almost like an iron line in that cornea. I’m not sure if that is a Fleischer ring as that eye technically doesn’t have KC anymore and he said “line” and not “ring,” but I didn’t think to ask at the time and he sounded a little stumped by it.
Also, the tech had me read the Snellen chart with my lenses in—or with correction—but then forgot to have me reread it with my lenses out. Therefore, I have no idea what my actual VA really is, but with great difficulty, I could read 20/30 in each eye and a poor 20/25 with both eyes with correction. Mind you, I can barely wear my sclerals due to severely dry eyes, so I live in ghost-y land the rest of the time. In the right lighting, I’d maybe believe I’m a weird 20/30 with my sclerals, but my near vision is still terrible and if any bright light is around, I tend to get the whiteout effect, holes in my vision, pain, and all sorts of bizarre things. When I got my final pair of scleral lenses in September from my optometrist, my corrected VA was 20/20 in my right eye and 20/30 in my left due to the opacity, so I have lost a line in the former eye with correction and much more without.
Therein lies the problem. Per my topographies over the last 18 months, the severity of KC in my right eye dropped from 76% to 32%. My K-readings, which measure the curvature of the corneas at various spots, have gone down from 51 diopters to 48 diopters at the steepest area, and if you look at my colorful topographies, the pink area (very bad) is now gone and the red area (bad) is extremely small. It’s improved since this time last year, in fact. Now, my CXL surgeon told me, “If you get improvement after cross-linking, you’ll continue to improve for the rest of your life.” Per my scans, it sure seems that is the case and that I’m the poster child of CXL, yet my vision in the keratoconic eye is getting worse—and it’s in terms of ghosting, which should mean an increase, not a decrease, in my irregular astigmatism: the hallmark of keratoconus.
My ophthalmologist was clearly mulling over this and throwing out theories. He wondered if the Ehlers-Danlos was causing changes to the shape of my eye’s lens, which would definitely create wonky vision, but I don’t think he had a test for that. And so in the end when the exam was complete, I got the monkey scratching his head while telling me, “Your eyes really do look good,” which brought back that old memory of the note from my former internist about looking good on paper.
If it took me a decade to figure out Ehlers-Danlos syndrome was what had turned me into the walking dead, should I pay more attention to this oddity with my eye that looks good—minus the keratoconus, etc., etc.—as well?
At this point, I feel like a monkey scratching my head, too.
A FALSE ALARM, BUT KEEP YOUR SEATBELTS SECURELY FASTENED

Image Source: http://www.seatmaestro.com
I don’t like to fly. I get extreme anxiety and have had full-blown panic attacks at every elevation imaginable, even after taking a fear of flying course nearly 20 years ago. So, when I went to see my optometrist a couple of weeks ago to find out why my vision was worse and more ghosted in my right eye, I had that fear-of-flying feeling the whole time: being completely out of control and waiting to crash and burn at any second. After all, if I’m not holding that plane up, then who is?
As usual, an assistant had me read the Snellen chart—a useless tool for assessing the visual acuity (VA) in anyone with keratoconus (KC). I just wanted to know how much my VA had changed in my right eye. Well, this woman didn’t want to tell me, but I do know that the VA in my left eye was unchanged because I turned around and read it on the wall when she walked out and saw 20/60 written next to the letters. I couldn’t see that while staring straight at it in the mirror. Again, the Snellen chart is worthless and there is no way I really have 20/60 vision in my formerly better eye pre-op and then formerly worse eye post-op. I didn’t get near that line with my right eye, so I believe I lost around 4 lines of vision over a month in that eye. I’m sure that sounds impossible, but I was progressing so quickly pre-op that it really is possible. I had that awful feeling of sitting in a plane knowing we would be taking off very shortly.
Next, I had to have the dreaded corneal topography done, as that is the gold standard for diagnosing and tracking KC. I looked into the machine and stared at a tiny hot air balloon that I saw multiples of with each eye while a photo was taken. My fate was sealed, just like when they close the door to the plane.
We headed back to the exam room and I waited for my doctor with my heart pounding. What did the topography show? Was I progressing 13 months after collagen cross-linking (CXL)? Why doesn’t anyone research people who get keratoconus from Ehlers-Danlos syndrome?
My doctor came in and he knew why I was there as we had spoken on the phone, which is a rarity in the States. He looked over a few things on the computer and then my topographies came up, but I couldn’t see them in detail. I think he spent 20 seconds comparing them to my previous ones from this June, but it felt like 20 minutes and I could hear those huge, jet engines starting up: the clear sign of impending doom.
Finally, he spoke and said that there was no difference between my topographies. I actually cried right there in the exam room out of relief, which is how I feel when a plane firmly touches down on the runway. I was horribly embarrassed and it only lasted 5 seconds and I wiped my eyes and apologized. But, what was wrong with my eye?
My doctor checked my eyes and looked to see if the slight scar I have in the right eye was worse, but it wasn’t. Another thing that can initially cause ghosted vision is a cataract, which may be a side-effect of CXL due to the UV light, but my lens was clear. He thought everything else looked normal in both eyes, aside from the scar partially blocking my vision in my left eye from CXL.
He decided to do a refraction and apparently my prescription has totally changed since I saw him a few months ago, but not for the worse. I’m still confused on what that means exactly, but that is precisely what he told me and I wish I had gotten copies of my refractions, but you have to pay for records. I can still drive with my scleral contact lenses, but either due to the sun or the lights at night it’s really hard. As I rarely wear them due to the pain, I noticed that my vision had gotten worse without my lenses in, which is the bulk of the time.
I told my doctor again my concerns about CXL lasting due to Ehlers-Danlos. He told me that he had no idea about that or what was wrong and that I had surgery that totally effed up my eyes—that would be both eyes due to the prescription change and yes, I cleaned up his language. What did he mean by “effed up my eyes?” I believe he was referring to the fact that my corneas are changed at the molecular level, not truly effed up, but maybe a casual relationship with a doctor isn’t as great as I thought. He said that maybe my left eye had gotten better, but I’d been doing the cover-one-eye-and-then-the-other test for weeks and just looked at him like he was yet another inept doctor in this city. The free fall was starting.
I can’t even read on my hugely blown-up laptop with my right eye, so that is the one that is worse. That was my better eye 6 weeks ago and I was also right eye dominant due to that, so my visual acuity was based on that eye which used to read the 20/40 line with great difficulty, but previously read 20/100 pre-CXL. I am now left eye dominant as my brain is trying to compensate for the vision loss in my right eye. Do I need to have fancy initials after my name to figure that out?
Again, the Snellen-based VA means nothing with KC as you can get a driver’s license with 20/40 vision and I flunked the test almost 2 years ago when the KC was starting in my left eye and I could read 20/30 from that eye without correction. I got a license as I could get enough correction with glasses in my better eye to read it back then, but I have a huge restriction stating that I am blind in my right eye, which was at 20/60 at that time: my current VA. Legally blind is defined as 20/200 in the States; I rest my case on the idiotic Snellen chart.
So, my optometrist doesn’t know what is wrong or if the CXL will continue to halt the progression of keratoconus. Oh, he called it keratoconus three times so I’m going back to that. A Google search for “secondary corneal ectasia from Ehlers-Danlos syndrome” yields zero results, unless my posts come up, so keratoconus it is. Many disorders are associated with KC and until the medical world catches up and comes up with new names, I’m staying in the KC club. My topographies give a diagnosis of keratoconus and the big specialist who did my CXL had no clue I had Ehlers-Danlos syndrome, although I did mention the fact that I thought I might have it and he told me to see a geneticist. If the only real difference is the typical age of onset and the lack of disease burn-out, I’m sticking with keratoconus and not changing my tag line.
What is wrong with my eyes again? My vision is a bit better today so I wrote this post. Who effing knows? The plane crashed and there are no survivors. I’ll post an update when they recover the black boxes.
IMPENDING DOOM: MY VISION IS WORSE & ALL ABOUT MY PSEUDO-KERATOCONUS
Photo Source: 40ans.ehess.fr
I was in deep thought about my collagen cross-linking (CXL) surgery awhile ago. I’ve read every journal article online about epi-off CXL, poured over the interviews with the top surgeons and their speculations on whether CXL will last in the long-term for keratoconus (KC), and thought about everything my top-notch surgeon told me at my pre-op appointment about the efficacy of CXL.
Since epi-off CXL was first performed in Dresden, Germany in 1998, the studies have shown there is no progression of KC and in the small percentage of people who don’t benefit from CXL from the get-go, it is effective when the surgery is repeated. This abstract from 2006, while not long-term, demonstrates the halt in progression. So, why was I worried?
Well, it wasn’t until I found my great optometrist this summer that I learned that although I look like I have KC per my scans and tests, my vision is that of someone with keratoconus, and despite all of the medical literature stating that keratoconus, a primary corneal ectasia, or thinning, can be caused by Ehlers-Danlos syndrome (EDS)—I really have secondary corneal ectasia caused by EDS. Should I change the tagline on my blog? As my optometrist stated, “It’s the same thing more or less.”
Per the “more or less,” here are the differences:
The true cause of KC is not known but there is a connection, at least in part, to faulty collagen in the cornea, but KCers don’t have a systemic disease that causes faulty collagen throughout the body like EDS does. A dry abstract discussing collagen fibrils in KC.
KC tends to show up in one’s teens or early 20s and runs a course of progression before burning out—usually within 20 years. With my secondary corneal ectasia, which apparently has never been researched, there is obviously no burn-out cycle as my body will continue to produce faulty collagen V for the rest of my life due to EDS type II. Therein lies the big problem, or so I think.
With CXL, the weak collagen fibrils in the cornea are tightened up by creating cross-links, much like adding rungs to a ladder. That sounds like a win-win for true KCers and for me. By creating all the cross-links, the cornea is stiffened and aged in essence (see abstract), which burns out the KC as cross-linking and stiffening are naturally occurring processes in normal, aged corneas. That’s good for KCers and in my mind, has no affect on my ectasia with no burn-out cycle and continued production of faulty collagen.
So, why all the worry again? I began to think about cell turnover. Most of the cells in our body turnover in time. What would happen to those nice, cross-linked collagen fibrils when the cells in my cornea, or within the stroma more precisely, turned over? With true KCers, I don’t think it matters as the disease has burned out, but for me, I believe that all the good collagen fibrils will be replaced by the old and it will only be a matter of time before the pseudo-keratoconus—what I’m calling this disease—shows up again.
Then, what are the options? I see none. When KC is severe enough, corneal transplants are the only option, but they reject sooner or later and the healing process is very long. I also have abnormal connective tissue due to EDS, which would make finding a match rather difficult, but that’s an assumption. Lastly, transplanted corneas in KCers who are still progressing can occasionally develop keratoconus again since the disease process is still active. I believe that would be a huge cause for concern in my case due to my faulty collagen production, not to mention my healing and scarring issues from EDS which would make transplants so problematic. A single case report highlighting the recurrence of keratoconus post-transplant.
Now, I was just thinking about all of this and then I noticed my vision got worse all of a sudden, rather like when I first noticed the psuedo-keratoconus. I thought it was from the sclerals I have to wear a few times a week to drive and that it would go away in a couple of days, per usual. That was about a month ago, so it’s not from wearing the sclerals. I don’t have any symptoms aside from more ghosting in my right eye, which was my better eye post-CXL. Now, my left eye with the scar is the better eye and my brain has made that the dominant eye. As the vision in my right eye is worse than the left, it means I’ve lost more than 2 lines of vision in a month or so, which is how this whole debacle started by losing a line every 4-6 weeks on the Snellen chart.
I did have a lot of testing at my 1-year follow-up in late September for the FDA clinical trial, but due to my corneal specialist being the worst ophthalmologist known to humankind, he came into the room for 30 seconds and didn’t say a thing. The reports, which are required by the FDA, never seem to make it to my surgeon in L.A., so who knows if anyone even reviewed them. No one told me anything was awry and I had no reason to suspect anything at the time. I do remember that my VA was the same, not that they’re very accurate at that practice or that it truly represents keratoconic vision.
I spoke with my optometrist about my eye and my concerns and have an appointment next week for an eye exam and corneal topography to see if there is progression. The CXL did work as I got 6 lines of vision back, which is very rare as most get 1 to 2 lines back or none at all. I do know that the cell turnover of the collagen in the stroma is several years and I’m shy of that at about 1 year post-op, but I have no idea what else it could be unless the very mild scar I have in my right eye that’s been stable for 8 months suddenly went wild, in which case I still won’t get my former vision back, and that’s all I want right now, even though most people would be crying in the corner if they had to see the world through my eyes.
I wish I could just get a break and I had to pay so much money for CXL that I didn’t have—I’m sure more than most Americans have in their savings account. When I had the talk with my optometrist about my concerns with CXL, EDS, and the pseudo-keratoconus, he agreed and said, “It’s a whole other monster.” Why didn’t he say that the first time? Maybe they could state that in the medical literature: that a condition that looks, but doesn’t exactly act, like keratoconus can be caused by EDS and it’s a whole other monster, rather than stating that keratoconus can be caused by EDS, period. Perhaps the inept corneal specialist who has M.D. after his name could have told me that after I was diagnosed with Ehlers-Danlos syndrome.
I also found out from my optometrist that if I had had an EDS diagnosis in September of 2012 when I had CXL, instead of in November, that I would have been excluded from the clinical trials. That’s doing wonders to quell my nerves while I sit and twiddle my thumbs and ponder writing a letter to the German ophthalmologist who developed CXL to get his take on its efficacy on my pseudo-keratoconus.
Theo Seiler, M.D., Ph.D., the creator of CXL who also looks exactly like my late grandfather. Hmmm…
Photo Source: http://www.meaco.org
20/40 = VISUALLY IMPAIRED?

Photo Source: http://www.ennovation.com
I had near-perfect vision less than 2 years ago. It was somewhere close to 20/20, aside from some mild myopia, or nearsightedness, that I had developed in my early 20s and did not even wear glasses for.
Then, the keratoconus (KC) developed and went wild and you can read my blog for that saga. I was at my corneal specialist’s recently as he wanted to see me for a 6 week follow-up after discovering central corneal opacity, or scarring, in my right eye months after my bilateral cross-linking (CXL) surgery.
Despite what I have felt has been rather negligent care, I got the full workup at the appointment: reading 2 eye charts, a refraction, a corneal topography, a corneal pachymetry, a check of my ocular pressure, and who knows what else I forgot. I was in a bad mood due to the disorganized clinic and was not really sure why I needed all the tests when I just had them done, but asked if I could at least have a copy of my topographies since nothing was initially sent to my CXL surgeon in L.A. for the clinical trial.
The techs are nice and had no problem with my request of having 4 papers copied, as opposed to the last time when I asked the front desk girl, who said she would have to charge me. Now, I finally had the scans I needed to see what my corneas and KC really look like at this stage, although my surgeon confirmed the other week that per my scans, the CXL was successful in both eyes and the progression of KC has been stopped in its tracks. Thank the Lord for modern medicine.
After all the testing and finally seeing what I could of those scans myself, the doctor rushed in talking a million miles a minute. He never seems to remember who I am or what my post-op issues are, which is really frustrating. He asked if I had any improvement since I had last seen him and I replied that I had some intermittent watering in my left eye—possibly due to the Restasis starting to work after 5 months—and that my right eye with the scarring had the same vision, which is a good sign, as well as the fact that the horrid light sensitivity (sun burning my retinas) was better, but not gone. He did a quick check of my eyes and said, “Good. Good.” That told me nothing, per usual, so I began with the questions that he hates, as he is already making notes in my chart at this point.
Here we go with the issues to preface all this. I read 2 eye charts—from right to left my visual acuity (VA) is now 20/40, 20/40 on one chart and 20/30, 20/40 on another. My left eye had gone up to 20/60 at my last appointment, so I was dealing with a post-op fluctuation that has cleared up. To err on the side of caution, I will say my vision is 20/40 with great difficulty on those last 2 lines, as no one has had me read the charts with both eyes, or binocular vision, which often gives a better VA. Would my true visual acuity not be of importance post-CXL? Well, of course, but I am dealing with sub par healthcare here. However, the big question is: why can I not see?
I should add that I do have a bizarre zone where I can see somewhat normally—it seems to start 1 foot in front of me and stop at 4 feet or so and there can be no sunlight or bright, artificial lights or the whiteout sets in. This is the safe zone and aside from a plasma-type TV on a not-too-far wall, I get staggered vision of everything outside that space in small rooms. For a description of how I see outside, in big spaces, and in the world in general—also known as the Ghosted Mess—refer to this post.
I have to ease my way into questions or my doctor gets irritated and the appointment ends, so I started with the basics. I wanted to know if the Restasis was causing the intermittent watering in my left eye, or if that was just from my corneas finally starting to heal from the surgery, as Ehlers-Danlos syndrome (EDS) is causing very poor and slow wound healing. The doctor could not answer that one. He kept saying my eyes were dry due to my meibomitis (MGD), which causes a lack of lipid (oil) layer in the tears, and that I just need more IPLs. I told him I had my last IPL 2 months ago and his associate—the doctor I like who specializes in dry eye—said more IPLs would do nothing at that point and I would not need a touch up for possibly a year.
I had 5 IPLs with no improvement that I noticed. However, the doctor thought they were successful in terms of the meibomitis, but as my eyes stopped producing the water layer in my tears post-op, they were still dry as a bone. Yes, this is all confusing, but for more information on MGD, as well as post-op dry eye, refer to this post. The corneal specialist gives me an odd look every time I explain that my complaints are related to my lack of a water layer and he says that I could barely open my eyes due to the meibomitis before the IPLs—although I only saw him once since 2010 and never had that symptom so I think he has me confused with another patient. Can I just see the dry eye specialist instead?
That leads to the big question—if my vision is roughly 20/40, why am I visually impaired? 20/40 vision is legal to drive in most, if not all, of the U.S. and I am not too sure I should even be on the road late at night, let alone left to wander in a big box store, which I would like to peruse with a stiff drink to offset the anxiety from the chaotic mess. Why do people look like shapes and colors and nothing more, unless they are in my safe zone? Well, the doctor is not sure, of course. What is he sure of? Why is he a doctor? Why is he the best corneal specialist in this horrid city? I may have better luck getting answers from the local fortune teller, who happens to be in the jenky strip mall next to my motel.
Now, I am not an ophthalmologist, but I am quite capable of interpreting my scans. Per the topographies, my better eye pre-op has no evidence of KC now in either the scan—showing no corneal steepening and 0% severity—or the K-readings, which are in the normal range now. My worse eye pre-op decreased in severity by 32.5%, although my K-readings are relatively the same in that eye, thus showing keratoconus—although it will not progress further due to CXL. K-readings measure the curvature of the cornea and there is still a significant steepening, which I can also see in the color-coded scan, but it appears to be much less severe, which makes no sense, especially since I got 6 or 7 lines of vision back in that eye. Both topographies do look quite different from my pre-CXL ones, which is rather fascinating. So, it would appear that I would have no keratoconic vision in my better eye, yet there is from my vantage point and I do not have my old 20/20 vision, regardless. May I also point out that at my last appointment, my doctor could not even tell me if the CXL had worked in that eye. Can I please move to L.A. with a giant dehumidifier and go see my surgeon for follow-ups instead? As mentioned, even I could interpret that scan with my impaired vision!
Back to the question at hand—my doctor asked when I would be seeing my surgeon again, as he seems to think I am able to go to L.A. at the drop of a hat—even though I would need an all day ride, have to pay a huge cash sum to see my doctor, and rent a motel room there, while living in one here. I reiterated for the 100th time that I have not seen him since my surgery in September of last year due to X, Y, and Z—not to mention that my local doctor referred me there and said he would handle all my follow ups. My patience was wearing thin.
Then, he asked how soon I could have laser vision correction surgery done there, even though that is my local doctor’s specialty (hence, corneal specialist). Is he crazy? I am 7 months post-op and a poorly healing, scarred mess due to my EDS and he thinks laser vision correction—namely PRK, which to my knowledge is still being studied for safety in post-CXL eyes (please fact check that), is a good idea? Due to the weak collagen structure in keratoconic corneas prior to the development of CXL, laser vision correction is contraindicated and is why all laser vision correction patients are given a topography to look for any evidence of KC before LASIK or PRK surgery. My eyes are so dangerously dry, plus the central corneal opacity that is no worse 6 weeks later but has not resolved, and he is even considering this? Furthermore, upon researching this issue just for the hell of it, the only scholarly, research articles regarding PRK following cross-linking involve or reference this ophthalmologist in Greece, who is on the payroll:
Financial Disclosures: Dr. Kanellopoulos is a consultant for Alcon, Inc., maker of the Wavelight excimer laser that he uses for topography-guided photorefractive keratectomy [PRK].
Article Source: http://www.aao.org/isrs/resources/outlook/11/01_11_feat.cfm
Maybe it is best to just see the local shaman wandering in the desert at this point. Perhaps some native shrub, like tumbleweed, can fix my vision—or is the local shaman in on the hustle to further destroy my corneas for some exorbitant fee, as well?
I told my doctor—who I now have absolutely no trust in—that there was no way I would go through surgery again with all the complications I have had and he mentioned something about my vision being bad from astigmatism. What astigmatism? Irregular astigmatism aka keratoconus? 9 months before my diagnosis, the optometrist I saw had misdiagnosed my keratoconus as mild astigmatism in my worse eye. Was this something new that my doctor pulled from the refraction done that day that I was not given a copy of? Add it to the list of copies I will be paying for very soon.
So, aside from residual keratoconic vision and little improvement in my K-readings in my worse eye, which I still don’t understand if the cone is so much flatter per the topography, is massive astigmatism in both eyes—the normal kind—contributing to the significant visual impairment now? If so, why can I not see any better with a refraction, just like when I had one before my diagnosis. I just answer, “Same” every time they flip the lens and ask, “Which is better—1 or 2?” Is the KC cancelling out any hope of lenses correcting the astigmatism? Why can I not get correction in my now non-keratoconic eye like my brother who has astigmatism and gets by fine with glasses? I am so utterly confused and Dr. Corneal Specialist is of no help.
As I have no choice but to wait and hope my vision improves a little more as my corneas continue to heal, patience has now been added to the survival box, and while I twiddle my thumbs, I will keep crunching the numbers in attempts to resolve the elusive mathematical equation involving my VA: 20/40 = X.
THE ART OF KVETCHING: HOW TO WORK THE AMERICAN HEALTHCARE SYSTEM
Image source: http://www.amazon.com
Some matters call for drastic measures. They require you to reach deep into your bag o’ tricks to find a resolution. For me, this is where being a kvetch, or a kvetcher, comes in handy.
For those not familiar, a kvetch is a complainer and kvetching is what a kvetch is always doing, although a kvetch can also kvetch, so it is both a noun and a verb. A kvetch also kvetches, which makes this even more confusing. Allow me to provide a quick lesson through some personal examples.
My father is always kvetching; he kvetches if his Diet Coke doesn’t come with a lemon wedge.
Don’t kvetch so much! I have something even worse to kvetch about.
Why is my grandmother such a kvetch? She’s the biggest kvetcher I know and doesn’t have a care in the world.
As the Yiddish spoken in America became Anglicized over the last century and the majority of American Yiddish-speakers of yesteryear have passed on, it’s all taken with a grain of kosher salt. Fancy Schmancy was not a phrase used in the old country, after all.
Nonetheless, the term kvetch is used in a derogatory sense and is generally reserved for those types who chronically complain about everything in a very drawn-out way. At the right time, however, I put on the kvetch hat and make the most of it. You must kvetch with an end goal in mind, or else you might as well be a plain old complainer. Kvetching is an art and one must know when and how to use this craft.
I had to pull out the kvetch hat quite recently in order to remedy a problem. Refer to my last post for the whole saga, but in short, my corneal specialist just left me hanging over a week ago with a diagnosis of central corneal opacity in one eye, a type of corneal scarring that can lead to blindness and is a rare complication of cross-linking (CXL), which I had done 6 months ago for my keratoconus. He told me I had to go back to L.A. to see my CXL surgeon, which isn’t possible, and that was that.
I have been self-treating my eye with 2 prescription drops I had on hand since the Friday I was diagnosed with the opacity and was awaiting a response from my CXL surgeon, which I got in due time via e-mail. He told me that it didn’t seem that serious—as opposed to my local doctor, the corneal specialist, who told me I could lose my vision in a few weeks. He mentioned that he would be happy to see me, regardless. That got me nowhere since traveling to L.A. was out of the picture. Who was I to believe? I had to save my eye, so it was time to start kvetching, but to whom? This is not a solo sport.
Well, I got a second chance due to my local doctor’s assistant not reminding him at my appointment—despite reminding her—that this was my 6 month follow up for the FDA clinical trial and I would need the appropriate paperwork filled out and various tests done. My doctor didn’t do anything required by the FDA, so I was rescheduled to see the optometrist who works with the surgical patients this past Friday. That was just what I needed. A chance to perform the art of kvetching in all its finery.
In the meantime, I called the clinic the Monday following my disastrous appointment and left word for my doctor that I had contacted and heard back from my CXL surgeon, wanted to be treated with an ocular steroid and antibiotic and have a follow up in 6 weeks, and to have him call me back in regards to this. No call. I called again on Thursday afternoon and asked why he had not called back. The rude receptionist who answered told me, “Your message was very lengthy and he did get the message.” Perhaps he could get e-mail like my very busy CXL surgeon? Regardless, her response told me nothing other than that I was still left hanging and he wasn’t going to treat me. I let her know that I couldn’t go to L.A., he was my treating physician, and that I expected a call back in a not-so-nice-tone to mimic hers. This was more of a stern kvetch, kvetch, kvetch.
I got a voicemail from my doctor Friday morning, which was the next day, saying I needed to make sure to come in for my appointment with the optometrist that day, as well as a voicemail from the rude receptionist reiterating what he said and that my doctor would see me at the appointment, also. Maybe the kvetching was paying off? I called her back and told her that I’ve never missed an appointment and asked why these messages were being left, just to kvetch some more for kvetching’s sake. This was really just to add extra emphasis and be a pain in the ass, or more accurately, a pain in the tuchus.
I am always running almost-on-time due to my mess of a body from Ehlers-Danlos that is like the Tin Man from The Wizard of Oz, but I managed to print out the journal article written by my CXL surgeon with the case report and treatment protocol I was following for post-CXL central corneal opacity and also had a copy of his message from the e-mail in hand for the appointment. All bases covered. One must do this to be an effective kvetcher—kvetch in an informed manner and keep your eye on the goal.
I had been in a pissed off mood for a week due to this ordeal, so when the cheery front desk girl asked how I was doing when I checked-in, I didn’t give a nice response. Why lie? It was more of a kvetchy, I’d-be-better-if-my-doctor-gave-a-crap response, but she continued to act in an odd, overly nice way that I don’t normally see there. I took a mental note of that.
Luckily, one of the better techs called me back for the various tests I had to do and I started kvetching to him about my treatment there—or lack thereof—since he sees me often and is aware I am never like this at the clinic. I even told him, while he was making notes in my chart, that I was on the two new drops in one eye and was treating myself due to my doctor not willing to do so. Oy vey. Would he warn my doctor that a kvetch was in the clinic? I was betting on it.
The tech and I went into a little room to do the corneal topography and I felt someone rubbing my back. What the heck? I turned around and it was the front desk woman I normally deal with and know fairly well, so something was definitely going on. She had the sorry-you’re-dealing-with-this look, which wasn’t necessary, but gave me some reassurance that a resolution might be coming. How did she know?
Had the rude receptionist spread the word that I was a hugely dissatisfied, kvetching patient who could possibly be a yenta—a gossipy woman—and ruin my doctor’s reputation in this big-small-town in the Southwest? Did the 99.5% Latino, but primarily Latina, support staff have a hidden knowledge of Yiddish and its deeper meaning? Had they been throwing these words around all week in between English, Spanish, and Spanglish?
“Esa mujer que always está kvetching. Oy, I’m gonna go loca.”
All the better for me. Relax, I speak Spanish, was an expat in México, and love that America is a melting pot of cultures. Thanks to the Spanyidglish, the kvetching was definitely paying off.
From there, I was led to another room and told to wait for the optometrist. I planned on kvetching to him about the predicament I was in and asking for his advice while throwing my hands up in the air, rather than just shoving it down his throat. Again, there is an art to this all.
However, just as I sat down, my corneal specialist came in. I wasn’t expecting him yet, so I quickly prepared myself. I noticed he was more humble than usual and had a nicer demeanor, as his mood is unpredictable. Had he prepared himself, as well? I believe the yentas in the office had warned him about me, as well as the tech. I did kvetch about my predicament to an extent, but I was armed with the medical journal article and the e-mail message, all from my CXL surgeon. Perhaps this would finally be resolved. One must know precisely when to take the kvetch hat off, of course.
The optometrist quickly came in and now both doctors were tackling the opacity issue together and taking turns peering into my eye and talking in hushed tones. The optometrist could see the opacity but thought it wasn’t that worrisome for now. My specialist actually read the case report in the article I had presented and then agreed that the ocular steroid I was using was the best approach and said that he wanted to see me again in 6 weeks to recheck my eye. Was that not what I had asked for in the lengthy message? He even kept the journal article—fancy that! He reiterated that it would be best to go to L.A. as my surgeon has been doing CXL since the U.S. trials began, but my doctor is doing them now, so what will he do when this happens to one of his own CXL patients?
Who cares at this point? The kvetchy wheel got the grease again and that, my friends, is the whole megillah. What a never-ending story it is—similar to reading a long post written in three languages.
LOOKS LIKE I PICKED THE WRONG WEEK TO STOP SNIFFING GLUE
Photo Source: http://www.knowyourmeme.com
I don’t want to write this post. I had a preliminary, uneventful post floating around in my head regarding my 6-month, post-CXL checkup, but then the crap hit the fan, which I think happens in Airplane, as well. Oh, I so wish that movie could have been on any of the boring channels of Dish I get at the motel last night.
Once again, I am left wondering how this happened when I’ve been at my ophthalmology clinic at least every month since my surgery. As I was in a clinical trial for cross-linking (CXL) for keratoconus (KC), I have had post-op checkups at 1 week, 3 months, and then 6 months, which was yesterday. These are all done with my local corneal specialist.
However, due to the IPL treatments I’ve had every month or so for meibomitis, I have been seen more often by a different associate at the clinic. Since I pay cash for the IPLs and they bill insurance for the office visit, could he not do a 1 minute exam of my corneas to make sure all is well due to my status as a post-op patient? I also mentioned to both doctors I see there that I was diagnosed with Ehlers-Danlos syndrome (EDS) this winter, which due to poor wound healing, should have led to more frequent post-op checkups due to the complications I already had.
I went in yesterday afternoon expecting to wait hours for my usual 5 minute appointment, get no answers as to why my eyes are still so dry and the sun is still burning my retinas, read a big, lighted board with lots of letters for the FDA, and call it a day. Things started out fairly well. With great struggle, my visual acuity (VA) is largely the same. From right to left, I came in at 20/40 and 20/50. The 20/50 eye was 20/40 last month, but it fluctuates and this technician isn’t my favorite. I wasn’t worried, and that was my better eye pre-op. The fact that my bad eye is still holding at 20/40 when it was 20/100 pre-CXL is atypical and great news.
My doctor checked my eyes for dryness first. He said that my eyes were a 5 on the dryness scale due to the IPLs and possibly the Restasis and were around a 12 before—is that the 1-10 scale and was 12 added for emphasis? He noted dry spots on my left cornea, which was my better eye dry-wise and keratoconus-wise. Well, that’s strange. I was just wondering how I’m a 5 with no tears and mentioned I had ointment and liquid gel drops in my eyes, but he said he can see beyond that. That didn’t answer my question really, but I figured that this too shall pass.
Then his assistant put the yellow drops in my eyes and maybe another drop and then he did an in-depth corneal exam. It seemed all was well, until he stopped and told me I had central corneal opacity and a scar forming in my right cornea, or something along those lines, as I tend to experience hearing loss at times like this. At least he was talking and giving me more than 5 minutes this visit, so I asked what that meant as it didn’t sound good. He told me there was cloudiness in my cornea and something about a scar and that I needed to see my Top Doc CXL surgeon in L.A. He said, “When can you go… 2 weeks, 4 weeks?” Oh, this wasn’t good at all. Here is why:
Corneal opacity is a disorder of the cornea, the transparent structure on the front of the eyeball, which can cause serious vision problems. Corneal opacity occurs when the cornea becomes scarred. This stops light from passing through the cornea to the retina and may cause the cornea to appear white or clouded over.
There are many causes of corneal opacity. In some cases, your doctor can recommend a treatment that will reverse the opacity and lessen your chance of needing additional treatment, such as surgery.
Article Source: www.http://www.med.nyu.edu/content?ChunkIID=102906
I just kept staring at him, and the gears in my head were going wild. CXL is very safe, I saw the best surgeon, and my right eye, which was the bad eye, was not in the advanced stage or super-severe stage of keratoconus. If it were, I would have been disqualified from the clinical trial and my surgeon would never have taken the risk and done a corneal transplant instead. Nothing was making sense. Would I get a blind, milky-white eye like that 200-year-old jihadist that died awhile back? I thought keratoconus was bad enough?
I told him there was no way I could get back to L.A. again. I asked if he could send a letter and maybe my surgeon could explain what was going on from that and a record of my exam, but my doctor said he really needed to see my eye, but would send a letter, regardless. Forget the rides, the hotel, and paying cash to see the out-of-network surgeon who I had to sell a kidney for to get the bilateral CXL—now I’m having some possibly serious complication from my EDS as I have a heart murmur that has always been asymptomatic. I can’t see a cardiologist until the end of March and am hardly able to walk around the grocery store due to shortness of breath and horrid fatigue, which seems to be caused from the heart palpitations and regurgitation. This was enough worry for one month and now this?
I came back from the appointment in a state of shock and sent a 1,000 word count e-mail to my CXL surgeon, who luckily gave me his e-mail address months ago—fairly sure he’s regretting that one. I stayed up all night scouring scholarly articles in medical journals to try to understand this. I found a few things worth noting. Eyes with very thin and very steep corneas are more at risk of central corneal opacity and scarring. In one study, 8.6% of eyes developed significant scarring within 1 year post-CXL as a result of this.
A dry article discussing
My right eye wasn’t as advanced as these eyes steepness-wise per my topography and my surgeon’s remarks and although I have no record of my corneal thickness, it still made little sense. Could the EDS be behind it? I have type II and have tissue fragility, poor wound healing, and terrible scarring from incisions, although I didn’t have any incisions with CXL. Why did this happen then?
I found one study indicating that patients who developed central corneal opacity and scarring had complete resolution within 1 year, but now the article is hiding in Google somewhere. I don’t recall the problem was connected to thin or steep corneas, either. I have to dig pretty deep to find these and forgot to leave bread crumbs for that article, which would be called bookmarking it. Great. That was my big ray of hope, and don’t ask me how a scar resolves.
Regardless, some of these studies were older and with any new technology, one makes improvements. There is now a protocol using a hypotonic riboflavin solution along with the standard riboflavin solution to plump up the cornea during CXL to prevent opacity and scarring. It is also necessary to check for the flare to ensure the cornea is fully saturated with riboflavin and then to measure corneal thickness following that to avoid problems due to an overly thin cornea during the surgery.
Another dry article discussing this
Did my surgeon not do all that? I wrote about the flare in a past post, but I couldn’t remember anything about measurements and who knows what was going into my eyes? Why was I doubting one of the best keratoconus specialists in the world? Well, read my former post if you’d like to know why I don’t trust anyone with M.D. after their name.
Luckily, I found an article he wrote discussing the importance of all the above. Phew! Good doctor! I also read about a patient he had with the same problem, but shortly after CXL and they had vision issues from it. I presume I don’t since my VA hasn’t changed in that eye, not that I can see well due to the KC. He resolved it with long-term steroids and antibiotics. Hmmm…
Now, steroids (drops, pills, or whatever) make me very sick, and I’m still losing my hair from those following CXL, but according to the article, this is only 2 drops a day and in 1 eye versus 4 drops a day in 2 eyes post-op, thus 2 drops instead of 8 drops a day. Could I pull it off? I have a full bottle of the exact steroid he used on this patient, as my local doctor prescribed it for the dryness and I stopped it within 24 hours due to side effects, but I was on the 8 drops a day protocol. I even have a good antibiotic left over from my CXL. How is an antibiotic going to get contaminated—it’s fine. Why not?
So, as I am not one to sit around, like to be my own doctor and am damn good at it, would never be able to get a corneal transplant due to the EDS and cross-linked eye (yes, this appears to be causing rejection), and had a published treatment protocol to follow thanks to my surgeon, a medical journal, and Google—I whipped out my ocular steroid and ocular antibiotic last night and considered it treatment day #1. As a disclaimer, please do not follow any of my advise on playing doctor.
Oh Lord, tell me I don’t have to go to L.A. and that this protocol will work and not make me sick. I really picked the wrong week to stop sniffing glue, quit amphetamines, quit smoking, quit drinking…
Where’s a damn Blockbuster when you need one? It’s not like I can order Airplane from a motel room.
THE SUN IS BURNING MY RETINAS & OTHER POST-CXL OBSERVATIONS

Image Source: http://www.brooksidepress.org
It seems like it was just yesterday that I had bilateral, “epi-off” cross-linking (CXL), but I am just shy of 5 months post-op this week. My recovery has been beyond slow and rather atypical, so please don’t assume you will have the same issues. If you are having them and found my post, then great—there are more of us out there.
As I’ve mentioned in prior posts, I have an unusual form of KC that hits later in life and progresses extremely fast. Also note that thanks to keratoconus, which did have a silver lining, I was finally diagnosed with Ehlers-Danlos syndrome (EDS)—a genetic connective tissue disorder that presumably caused my KC and is also causing the slow healing.
Aside from the pesky dry eyes, which I wrote a whole post on, my biggest gripe at this point is with light sensitivity. It has slowly improved with time, but it just seems abnormal to be dealing with this problem still, although a fellow blogger who had her CXL around the same time as mine has the same issue still, too.
Following CXL, any light source was a problem and I saw sparklers and halos around anything that emitted light. Then there is glare, which I lump into the same category and is still a bit of an annoyance now. However, I recall not being able to even look into the silverware drawer the week I recuperated from CXL at my mother’s house. So, as long as I’m not dealing with glare from the sun, I won’t complain about trying to sort through my coins.
At this stage of the game, I have two big grievances with light sensitivity. The first involves using a computer due to the bright, white screen. For weeks after CXL, I couldn’t even open my laptop, but it’s still a nuisance now even if things are getting better. I’m not an IT person, but one of my fellow bloggers—who doesn’t even have KC—really helped me out with her comments. She suggested I adjust my screen’s brightness and other tips. Seriously, if you’ve never dealt with this, why would you think such an option existed on your computer?
Needless to say, one problem has been semi-resolved and I also learned I could blow up my entire operating system! That has been great since I can’t wear contacts still. If you have a PC, you can easily tinker around with your computer via Control Panel > Appearance and Personalization > Display (or at least that’s how it is in Windows 7 land).
My second issue involves seeing things outdoors during the day and driving. Regarding the latter, I can drive at night now although headlights are irritating, but I absolutely cannot drive in the day due to the sun. I live in the desert SW of the U.S. and the sun is usually a big ball of intense light, even though it’s freezing cold now. I get a “whiteout” effect—almost as if I were constantly driving west as the sun were setting.
The other odd thing is that while I’ve had this massive improvement in my visual acuity, I have typical, keratoconus vision with ghosting outside in daylight, which just adds to my reluctance to drive. This has improved drastically too, but before CXL, I could get one good drive in 1st thing in the day. After that, I shouldn’t have even been on the road.
I am still healing and my vision is still fluctuating a bit, but I have stable vision throughout the day due to the cross-linking and that is wonderful. I also am noticing that I am starting to be able to read some “fine print” on things, although if it’s too small I struggle and get a headache between my eyes.
While my visual acuity jumped to 20/400 post-CXL, I’m currently at about 20/40 in both eyes, although that last line is a struggle to read. Pre-CXL, I had monocular vision and was only using my better eye—now my slightly worse eye, which was at 20/60 and rapidly progressing like my other eye, which was no longer functioning. Sort of confusing. I wish I could explain it all in diopters, but the clinical trial follow-ups don’t seem to include a refraction.
So, aside from the horribly dry eyes, my hair that is still falling out from the steroid drops months after stopping them, and the light sensitivity and inability to drive a car during the day (huge problem!)—I am so glad I was able to max out my credit card and be one of the lucky few to get into a CXL clinical trial in the good ol’ US of A.
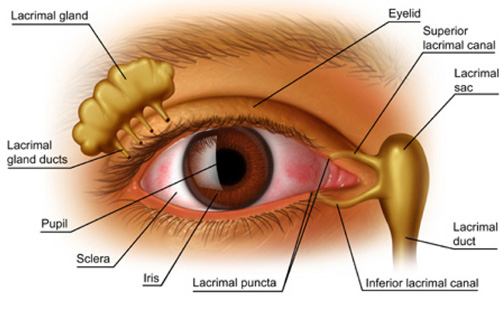
DRY EYES WITH NO END IN SIGHT
Image Source: http://www.holickieyecenter.com
Will my eyes ever have tears again? Does anyone know the agony of having eyes that are as dry as a bone? Am I the only one who has had this adverse side-effect from epi-off collagen cross-linking (CXL)? Why can’t I find any answers, even from my doctor nearly 4 months post-surgery? Will I spend my life with onions taped under my eyes to get them to water?
Let me preface this by saying that I had a dry eye problem before I developed keratoconus. Six years ago my eyes became very dry and I was having symptoms such as burning, irritation, pain, infections, my eyes being “glued” together in the morning, and whatnot. I ultimately was referred to my current ophthalmologist 5 years ago and after a thorough exam, he told me I had severe meibomitis and it could lead to corneal ulcers if we didn’t get it under control. I had what?
Along the margin of the lids there are a series of small sebaceous glands called the meibomian glands. They create and distribute an oily substance called lipids. Meibomian gland secretions help keep the eye moist and protect the tear film from evaporation. Upon blinking the upper lid comes down presses on the oil and pulls a sheet of oil upwards coating the tear layer beneath to keep it from evaporating. Meibomitis refers to dysfunction and inflammation of these glands. Oil production by the glands decreases and the oils that are produced become thicker (looking like toothpaste). The reduction in the quantity and quality of the oily layer causes the tears to evaporate more rapidly and this leads to symptoms of dryness burning and irritation especially upon awakening.
Article Source: https://www.eyeconx.net/wiki/mediawiki-1.15.1/index.php?title=Meibomitis
So, for the past 5 years I was on one protocol and drug after the next to try to control the meibomitis. Nothing really helped and I just dealt with it. Since meibomitis affects the lipid, or oil, layer of the tears (see the diagram above), it made my tears too watery, which is very different from my current complaint. As a result, I had “dry eyes” that watered to the point that tears ran down my face. This is because I essentially had no lipid layer (oil) in my tear film to give it viscosity. How ironic and irritating, but boy do watery eyes sound good right now.
Somewhere between dealing with the meibomitis and the freshly diagnosed keratoconus, a new ophthalmologist started practicing at my clinic. Due to my upcoming CXL last September, I decided to make my doctor happy and get a new treatment for meibomitis called IPL (intense pulse light), which is normally used for dermatological conditions. This new doctor was going to be doing the IPL procedures and I booked an appointment, even though it’s not covered by insurance.
This is where 2 brains are better than 1. He disagreed with every treatment my regular doctor was doing since I also have rosacea and it had spread to my eyes. Ocular rosacea can cause meibomitis and doing things like putting hot compresses on your eyes twice daily makes any type of rosacea worse it seems. IPLs were the way to go. Here’s how this fascinating, yet rather painful and nasty treatment works.
MGD [meibomitis] treatments with IPL equipment select a narrow band of light wavelengths (500-800 nm) to produce heat on the skin of the eyelids. The minuscule blood vessels directly under the epidermis take in the light and as their temperature rises, the congealed secretions of the meibomian glands begin to melt and the glands open up. The doctor then applies some pressure on the glands to remove all the troublesome secretions. The heat also drives out skin and eyelid microbes, such as parasites and bacteria that can exacerbate MGD [meibomitis]. If you think of the time-tested warm compress, you’ll find the IPL device is essentially its high-tech version.
Article Source: http://EzineArticles.com/6050685
The new doctor gave me my first IPL treatment 1 month before my CXL surgery. He thought I would be a great candidate for IPL due to having ocular rosacea, fair skin, and dark hair. I thought I had won the jackpot for once. Normally, results aren’t noticed after the 1st treatment, but I did notice some improvement in my tear quality. Oh, I was so excited! Then I had the CXL and the water layer of my tears disappeared. I’m also having a very slow recovery, which I presume is due to poor wound healing related to Ehlers-Danlos syndrome, but why is no one familiar with this problem? Am I really the only one?
Since my surgery, I’ve had 2 more IPLs with more on the way, all 4 tear ducts plugged (already had 2 plugged), used every artificial tear known to man, had a chronic rash under my eyes from the aforementioned drops spilling out of my plugged up eyes, and gone through at least 35 tubes of eye ointment and gel, which is what I’ve resorted to in order to keep my eyes moist. It looks great having all this goop in your eyes, by the way. Now my doctor has me on Restasis® drops, which I had resisted for 5 years. The active ingredient is cyclosporine.
The immunosuppressive effect of ciclosporin [cyclosporine] was discovered on 31 January 1972. In addition to transplants, ciclosporin [cyclosporine] is also used in psoriasis…and, infrequently, in rheumatoid arthritis and related diseases, although it is only used in severe cases. It is commonly prescribed in the US as an ophthalmic emulsion for the treatment of dry eyes.
Article source: http://en.wikipedia.org/wiki/Ciclosporin
From the manufacturer:
RESTASIS® Ophthalmic Emulsion is a prescription medicine that helps increase your eyes’ natural ability to produce tears, which may be reduced by inflammation due to Chronic Dry Eye.
Article Source: http://www.restasis.com
It usually takes 3-6 months to even see if it works and is not cheap, even with insurance. Due to side-effects from Restasis®, my eyes are red and irritated, full of broken blood vessels, and burn all the time. I’ve been on it for 1 month with no results and after the continuing nightmare of my hair falling out due to the ocular steroids post-CXL, I’m wondering what Restasis® is doing to my body?
One benefit, unless it’s my imagination, is that I can eat spinach again. I normally would scratch myself silly after eating even a leaf of spinach. Is it a miracle cure for my plethora of food allergies? Speaking of food, I tend to eat a Mediterranean diet and am wondering if I can just ditch Western medicine, sterilize my 5-star olive oil, and pour it directly into my eyes?
Please don’t try this at home.
I’M TURNING INTO MS. BIGGLESWORTH

Photo Source: http://sr.photos2.fotosearch.com/bthumb/CSP/CSP097/k0974598.jpg
Three weeks ago, or nine weeks after my cross-linking surgery, I started to notice more hair than normal in the shower. Then I noticed clumps of hair in my wide tooth comb. Soon enough, the drain in the tub began to clog until I opened it up and found the mother of all hairballs.
Now, I’ve had this happen before. When I first got sick in 2001 with what I was told was fibromyalgia—stay tuned for a possible misdiagnosis post* (see update), my hair started to do the same thing until I lost at least 1/2 of it, if not more. It finally stopped falling out but didn’t grow back to its original thickness until I finally forced a GP to put me on thyroid medication, as my TSH was borderline high. It eventually grew back, but fell out two more times (not as badly) when I switched doctors and they subsequently screwed up my thyroid by switching my medication. However, this round, my hair is not only falling out but also has this strange texture, which makes little sense considering my hair is finally getting long—nearly 3 years later—and has a lot of “old growth.”
I chalked it up to stress on my body from the CXL surgery (read my last post) or the stress of dealing with my mother pre- and post-op. That didn’t quite fit the bill when I realized I had pretty traumatic surgery both physically and mentally in 2006 and no hair loss. Hmmm… What could be the root cause? I always seem to diagnose every malady I have so I just kept focusing on everything “cross-linking.” Then it hit me like a ton of bricks (or a giant hairball) while I was trying to get my Carol’s Daughter shampoo and conditioner through my now beyond coarse, dry, and unruly hair—that was a plug for CD… Great for ethnic, curly hair. Anyway, it had to be the Pred Forte eye drops, also known as steroids.
I started those drops on day 5 with instructions to use them 4 x day until told to stop. Steroids are used after CXL to prevent hazing, which I got anyway, although it went away within 2 weeks. I cannot take steroids, so I was worried about that drug, but an eye drop? How much can get into your system? A lot. I instantly got the insomnia—even while on Ambien to sleep, the night sweats, and my chronic musculoskeletal pain was through the roof. I stuck it out for 17 days and got permission from my surgeon in L.A. to stop the drug. All side effects subsided, or so I thought.
After researching this tonight, it appears there’s a huge connection between steroids and hair loss—a lot of hair loss—and that it continues long after you stop them. I do know that it takes 3 months for hair that has fallen out of the follicle to actually grow—or fall—out of your head, so I really am hoping this will stop soon since I wasn’t on the steroid for that long. The odd thing is that it changes the texture of your hair and makes it coarse, dry, and frizzy, which would be my natural texture—plus curly, so it’s a hot mess right now. I do get a trim next week and hope more layering (I lost any guys reading this) will hide the thinning that is rather obvious with my dark hair and pale scalp. I can’t chop it off after nearly 3 years of growing it out!
I know this might all seem trivial, like for those on chemo or men who are going permanently bald, but I’m famous for my dark, thick, curly hair and at this point, it’s all I have going for me!